Short Bowel Syndrome (SBS) presents a unique set of challenges for those affected by it. This condition, often resulting from surgical removal or dysfunction of a significant portion of the small intestine, disrupts the body’s ability to absorb essential nutrients. For individuals living with SBS, maintaining proper nutrition can be a constant struggle, as their digestive systems are compromised, and traditional dietary approaches often fall short.
In the complex landscape of SBS management, Total Parenteral Nutrition (TPN) emerges as a vital lifeline. TPN is more than just a medical intervention; it’s a critical component of care that sustains and nourishes individuals with SBS, providing them with the nutrients they need to thrive.
Understanding Total Parenteral Nutrition (TPN)
Before delving into the role of TPN in SBS management, it’s essential to grasp what TPN entails. Total Parenteral Nutrition involves the intravenous delivery of essential nutrients, including carbohydrates, proteins, fats, vitamins, and minerals, directly into the bloodstream. This method bypasses the compromised digestive system, ensuring that the body receives the vital elements it needs, even when the small intestine’s capacity to absorb nutrients is severely impaired.
TPN as a Nutritional Lifeline for SBS Patients
For many individuals living with SBS, TPN becomes far more than a medical procedure; it becomes a nutritional lifeline. When the digestive system cannot fulfill its primary role of absorbing nutrients from food, TPN steps in to bridge the nutritional gap. It provides patients with the necessary building blocks for health, offering them not just sustenance but also the potential for recovery and a better quality of life.
Tailoring TPN to Individual Needs
One of the remarkable aspects of TPN is its customizability. TPN solutions are not one-size-fits-all; instead, they are meticulously tailored to meet the specific nutritional requirements of each SBS patient. This personalized approach ensures that patients receive the right balance of nutrients, vitamins, and minerals, addressing their unique conditions and needs.
Administering TPN Safely and Effectively
The administration of TPN is a complex process that demands precision and expertise. Healthcare providers work closely with SBS patients to ensure the safe and effective delivery of TPN. This collaboration involves carefully selecting the appropriate formula, monitoring nutrient levels, and addressing any potential complications to guarantee the patient’s well-being.
The Role of TPN in Patient Recovery
Beyond its role as a nutritional sustainer, TPN plays a pivotal role in patient recovery. It becomes especially crucial during periods of acute illness, post-surgery, or while awaiting surgical interventions like intestinal transplantation. TPN provides patients with the strength and nourishment needed to weather these challenging phases, facilitating a smoother journey towards recovery and improved health.
In this comprehensive guide, we will explore the multifaceted role of Total Parenteral Nutrition (TPN) in managing Short Bowel Syndrome (SBS). We will delve into the intricacies of TPN, its customization to individual needs, and the significant impact it has on patient recovery. Join us on this enlightening journey as we uncover the critical lifeline that TPN represents in the complex landscape of SBS management.
Section 1: Understanding Total Parenteral Nutrition (TPN)
Demystifying Total Parenteral Nutrition (TPN)
Total Parenteral Nutrition, commonly known as TPN, is a medical intervention that plays a pivotal role in the management of Short Bowel Syndrome (SBS). To grasp its significance, it’s essential to demystify what TPN involves. TPN is a method of delivering vital nutrients directly into the bloodstream, circumventing the digestive system entirely. This intravenous infusion provides the body with a balanced mixture of carbohydrates, proteins, fats, vitamins, and minerals, ensuring that the patient’s nutritional needs are met, even when the small intestine’s capacity to absorb nutrients is compromised.
When the Digestive System Falls Short
SBS, often resulting from surgical resection or dysfunction of a significant portion of the small intestine, disrupts the body’s digestive processes. The compromised intestinal function makes it challenging for individuals with SBS to extract essential nutrients from food through traditional means. This is where TPN steps in as a crucial solution. When the digestive system falls short, TPN bridges the nutritional gap, providing a lifeline of sustenance that is vital for health and well-being.
Section 2: TPN as a Nutritional Lifeline for SBS Patients
The Nutritional Lifeline
For many individuals living with SBS, TPN becomes more than just a medical procedure—it becomes a lifeline of nutrition. When the body’s natural mechanisms for absorbing nutrients are severely impaired, TPN steps in to fulfill this essential role. It provides patients with the necessary nutrients they need to maintain health, repair tissues, and support bodily functions.
Nourishment Beyond Sustenance
TPN goes beyond merely sustaining individuals with SBS; it offers the potential for recovery and an improved quality of life. By delivering a balanced and customized mixture of nutrients directly into the bloodstream, TPN provides the body with the building blocks it requires for healing and regeneration. This not only supports physical recovery but also enhances overall well-being.
Tailoring TPN to Individual Needs
One of the remarkable aspects of TPN is its individualized approach. TPN solutions are carefully tailored to meet the specific nutritional requirements of each SBS patient. The composition of TPN is adjusted based on factors such as the patient’s age, weight, medical history, and unique nutritional needs. This personalized approach ensures that patients receive the right balance of nutrients, vitamins, and minerals, addressing their specific conditions and optimizing their health.
Collaboration with Healthcare Providers
The administration of TPN is a collaborative effort between patients and healthcare providers. Together, they work to ensure the safe and effective delivery of TPN. Healthcare providers play a crucial role in selecting the appropriate TPN formula, monitoring nutrient levels, and addressing any potential complications that may arise, prioritizing the patient’s well-being throughout the process.
Section 3: Tailoring TPN to Individual Needs
Customizing TPN for Optimal Nutrition
Total Parenteral Nutrition (TPN) is not a one-size-fits-all solution; it is a highly customizable approach to meet the unique nutritional needs of each individual with Short Bowel Syndrome (SBS). This tailoring ensures that patients receive the precise balance of nutrients required to support their health and well-being.
Factors Influencing TPN Formulation
Several factors influence the formulation of TPN for an SBS patient:
- Medical History: Understanding the patient’s medical history, including the extent of intestinal resection and any underlying conditions, guides the selection of appropriate nutrients and vitamins.
- Nutritional Deficiencies: Identification of specific nutritional deficiencies through blood tests helps determine which nutrients need supplementation.
- Body Composition: Factors like weight, age, and body composition play a role in calibrating the composition of TPN.
- Energy Requirements: The patient’s energy expenditure is calculated to ensure they receive the necessary caloric intake.
Balancing Macronutrients
The balance of macronutrients—carbohydrates, proteins, and fats—is carefully calculated to meet the patient’s unique needs. Adjusting these components is crucial to address the challenges posed by SBS and optimize nutritional intake.
Section 4: Administering TPN Safely and Effectively
The Complexity of TPN Administration
The administration of TPN is a complex process that demands precision and expertise. This section explores the various aspects involved in delivering TPN safely and effectively.
The Role of Healthcare Providers
Collaboration with healthcare providers is paramount in TPN administration. They play a critical role in:
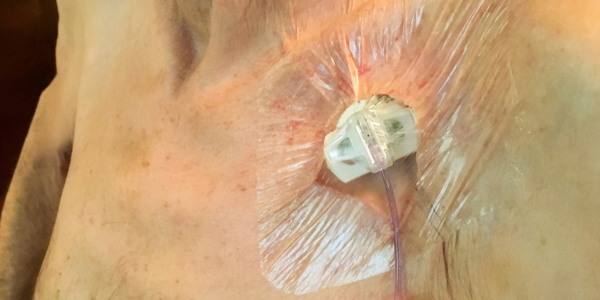
- Choosing the Right Formula: Healthcare providers select the appropriate TPN formula based on the patient’s individual requirements.
- Monitoring Nutrient Levels: Regular monitoring of nutrient levels through blood tests ensures that patients receive the correct nutrients in the right amounts.
Addressing Potential Complications
While TPN offers vital nutrition, it also comes with potential complications, including infection risk, catheter-related issues, and metabolic imbalances. Healthcare providers are vigilant in addressing and preventing these complications to ensure patient safety.
Patient Education and Empowerment
Patients are educated about the importance of adherence to the TPN regimen, proper care of the catheter site, and recognizing signs of complications. Empowering patients with knowledge is key to their active involvement in the safe administration of TPN.
Ongoing Monitoring and Adjustments
TPN administration is not static; it requires ongoing monitoring and adjustments. Regular evaluations, nutrient level checks, and collaboration with healthcare providers ensure that the TPN regimen remains effective and safe.
Section 4: The Importance of Staying Hydrated and Managing Fluid Intake
The Significance of Proper Hydration
Proper hydration is a fundamental aspect of managing Short Bowel Syndrome (SBS). Individuals with SBS face unique challenges when it comes to maintaining adequate hydration due to increased fluid loss through diarrhea. This section explores the importance of hydration and strategies for achieving a balance.
Balancing Fluid Intake
Individuals with SBS must carefully balance their fluid intake. While staying hydrated is essential, excessive fluid consumption can exacerbate diarrhea, leading to electrolyte imbalances and discomfort. Healthcare providers often work closely with patients to determine the right balance based on their specific SBS condition.
Signs of Dehydration
Being vigilant about recognizing signs of dehydration is crucial. These signs may include dark urine, dry mouth, increased thirst, and fatigue. Addressing dehydration promptly is essential to prevent complications and maintain overall well-being.
Managing Electrolyte Imbalances
SBS can disrupt the balance of electrolytes in the body, potentially leading to muscle cramps, weakness, and other complications. Regular monitoring of electrolyte levels and collaboration with healthcare providers are essential to manage and prevent these imbalances.

Section 5: The Role of TPN in Patient Recovery
Beyond Sustenance: TPN and Patient Recovery
Total Parenteral Nutrition (TPN) goes beyond providing sustenance for individuals with Short Bowel Syndrome (SBS); it plays a pivotal role in patient recovery. This section delves into the ways in which TPN supports individuals during critical phases of their journey.
Support during Acute Illness
During periods of acute illness, SBS patients may experience increased nutrient loss and challenges in maintaining adequate nutrition through oral intake. TPN offers crucial support during these times, ensuring that patients receive the essential nutrients necessary for recovery.
Pre- and Post-Surgery Support
Surgery is a significant aspect of SBS management, whether it’s for bowel lengthening or intestinal transplantation. TPN plays a vital role in preparing patients for surgery by optimizing their nutritional status and supporting post-surgical recovery.
Aiding in Intestinal Adaptation
For patients undergoing bowel lengthening procedures, TPN can aid in the process of intestinal adaptation. It provides a controlled source of nutrition while the intestine heals and adapts to increased functionality.
Enhancing Quality of Life
By addressing nutritional deficits and supporting recovery, TPN contributes to an enhanced quality of life for individuals with SBS. It allows patients to lead more active and fulfilling lives, free from the constraints of severe malnutrition.
Navigating SBS with TPN for a Brighter Future
Empowering SBS Patients through TPN and Hydration
The journey of managing Short Bowel Syndrome (SBS) is undeniably challenging, but it’s a journey that can be navigated with resilience and the right tools. In this comprehensive guide, we’ve explored the vital role of Total Parenteral Nutrition (TPN) and proper hydration in supporting individuals with SBS.
A Lifeline of Nutrition and Recovery
TPN emerges as a lifeline, providing essential nutrients when the digestive system falls short. It not only sustains but also aids in recovery during acute illness, pre- and post-surgery, and the process of intestinal adaptation. By bridging nutritional gaps and enhancing overall well-being, TPN offers individuals with SBS the promise of a brighter and healthier future.
Empower Your SBS Journey
We invite you to take an active role in your journey if you or a loved one has Short Bowel Syndrome:
- Consult a Healthcare Provider: Reach out to a healthcare provider or specialist experienced in SBS management to discuss your individualized treatment plan.
- Stay Hydrated: Maintain proper fluid balance by working closely with your healthcare team to find the right fluid intake for your specific condition.
- Join Support Communities: Connect with online support groups or organizations dedicated to SBS to share experiences, gain insights, and find additional resources.
To continue your journey of understanding and managing Short Bowel Syndrome and the role of TPN and hydration, explore these external resources:
- Short Bowel Syndrome Foundation: A valuable source of information, support, and community for individuals with SBS and their caregivers.
- American Gastroenterological Association – Short Bowel Syndrome: Provides comprehensive information on SBS, including treatment guidelines and resources.
- Oley Foundation: An organization dedicated to enriching the lives of those requiring home intravenous nutrition, including TPN.
As you embark on your journey with Short Bowel Syndrome, remember that you’re not alone. With the right support, knowledge, and determination, you can navigate the challenges and embrace a future filled with hope and improved health.