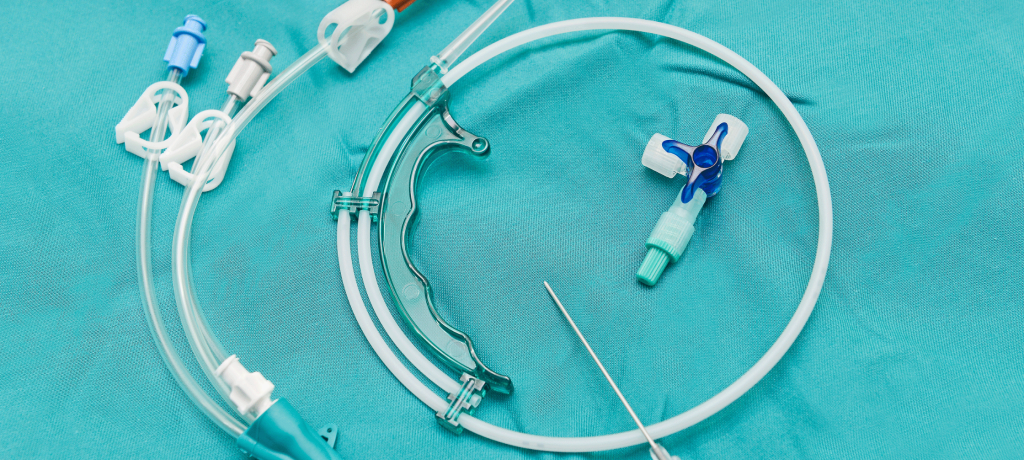
Central Venous Catheters (CVCs) stand as silent sentinels in the realm of modern medicine, bridging the gap between treatment and patient care with unwavering precision. These slender tubes, often inserted into large veins near the heart, have revolutionized healthcare by providing a direct conduit to the body’s central circulation. Through CVCs, healthcare professionals gain the means to deliver life-saving medications, fluids, and therapies, all while closely monitoring the patient’s hemodynamic status.
In the labyrinthine corridors of healthcare, CVCs are not a one-size-fits-all solution but a diverse array of devices, each meticulously designed to meet specific medical needs. From short-term catheters used for a brief stay in the hospital to long-term, tunnelled catheters that accompany patients through extended treatment regimens, understanding the nuances of these lifelines is paramount.
Yet, CVCs are not merely instruments of medical intervention; they are lifelines for patients grappling with complex conditions, providing access to life-sustaining treatments such as chemotherapy, parenteral nutrition, and hemodialysis. For healthcare providers, mastering the art of CVC placement, maintenance, and removal is a fundamental skill, ensuring that patients receive the best possible care while minimizing the risk of complications.
This comprehensive guide is a beacon of knowledge, illuminating the world of central venous catheters in intricate detail. We will explore the various types of CVCs, delving into their purposes and unique features. We will demystify the art of CVC placement, unraveling the intricacies of the procedure and the vital factors to consider. We will also delve into the essential practices of CVC care and maintenance, safeguarding both the catheter’s integrity and the patient’s well-being. Furthermore, we will discuss the art of CVC removal, a procedure that requires finesse to ensure a patient’s smooth transition towards recovery.
As we navigate the multifaceted realm of central venous catheters, our goal is to empower healthcare providers and patients alike with knowledge and understanding. Together, we will unlock the potential of these remarkable medical devices, appreciating their role as lifelines that bridge the gap between illness and healing. Join us on this journey through the intricacies of CVCs, where knowledge becomes a powerful tool for providing exceptional care and improving patient outcomes.
1: Types of Central Venous Catheters (CVCs)
A Spectrum of CVCs
The world of central venous catheters (CVCs) encompasses a spectrum of devices, each tailored to specific medical needs and clinical situations. Understanding the various types of CVCs is crucial for healthcare providers and patients alike. Let’s explore some of the most common types:
Peripherally Inserted Central Catheter (PICC)
Purpose: PICC lines are frequently used for long-term intravenous therapies such as chemotherapy, antibiotic administration, and parenteral nutrition. They are inserted through a peripheral vein, typically in the arm, and threaded into a larger central vein near the heart.
Advantages: PICCs are less invasive than other CVCs, making them suitable for outpatient settings. They offer a lower risk of complications and are often more comfortable for patients.
Non-Tunneled Central Venous Catheter
Purpose: Non-tunneled catheters are designed for short-term use, often in emergency situations or during surgeries. They are inserted directly into a central vein, usually in the neck or chest.
Advantages: These catheters provide rapid access to the central circulation but are typically used for a limited duration due to a higher risk of infection and complications.
Tunneled Catheters (e.g., Hickman and Broviac)
Purpose: Tunneled catheters are intended for long-term use, commonly in patients requiring frequent access for treatments like hemodialysis or chemotherapy. They are surgically inserted through a small incision, with a tunnel created under the skin to reduce infection risk.
Advantages: Tunneled catheters offer stability, reduced infection risk, and improved patient comfort during extended treatments.
Implantable Port
Purpose: Implantable ports are placed under the skin, usually in the chest area, for long-term use. They are accessed with a special needle for treatments like chemotherapy, reducing the need for visible external catheters.
Advantages: Implantable ports provide discreet access, reduced infection risk, and improved cosmetic outcomes, particularly important for patients receiving long-term therapies.
2: Placing Central Venous Catheters (CVCs)
The Art of CVC Placement
Placing a central venous catheter (CVC) is a skilled medical procedure that demands precision, knowledge, and a keen understanding of the patient’s specific clinical needs. The choice of CVC type and insertion site depends on factors such as the intended use, expected duration, and individual patient considerations.
Selecting the Appropriate CVC Type
Individualized Approach: The choice of CVC type should align with the patient’s medical requirements and treatment plan. Short-term therapies may necessitate non-tunneled catheters, while long-term treatments benefit from tunneled catheters or implantable ports.

Placement Site Selection
Central Vein Access: CVCs are typically inserted into central veins near the heart. Common access points include the subclavian vein, internal jugular vein, and femoral vein, with each having its advantages and considerations.
Sterile Technique and Infection Control
Strict Protocols: CVC placement demands scrupulous adherence to sterile techniques to minimize infection risks. Healthcare providers follow strict protocols, including hand hygiene, skin disinfection, and the use of sterile drapes and gloves.
Real-Time Imaging Guidance
Enhanced Precision: In some cases, real-time imaging techniques such as ultrasound or fluoroscopy may be employed to guide the catheter’s placement with precision, reducing the risk of complications.
Understanding the intricacies of CVC types and the meticulous steps involved in their placement is crucial for healthcare providers and patients alike. The decision-making process and procedure itself must prioritize patient safety and optimal treatment outcomes, ensuring that CVCs become lifelines to improved health and well-being.
3: Essential Care and Maintenance of Central Venous Catheters (CVCs)
Nurturing the Lifeline
Once a central venous catheter (CVC) is in place, proper care and maintenance become paramount to ensure its functionality, longevity, and the well-being of the patient. Let’s explore the essential practices for CVC care:
Dressing Changes and Sterile Technique
Routine Dressing Changes: The dressing covering the CVC insertion site must be changed regularly using strict sterile technique. This helps prevent infection and ensures a clean environment around the catheter.
Flushing and Medication Administration
Flushing: Regular flushing of the CVC with saline or heparin solution prevents occlusion and maintains catheter patency. Healthcare providers follow established protocols for flushing frequency and volume.
Medication Administration: Medications administered through the CVC must be compatible with the materials and lumens of the catheter to avoid complications.
Catheter Lumens and Line Management
Dedicated Lumens: Many CVCs have multiple lumens, each designated for specific purposes. Proper labeling and management of lumens ensure that the right medications and fluids are administered through the correct channels.
Prevention of Infection
Hand Hygiene: Healthcare providers and caregivers must practice rigorous hand hygiene before handling the CVC to reduce the risk of infection.
Site Assessment: Regular site assessment is critical to identify signs of infection or complications early. Prompt reporting of any abnormalities is essential for timely intervention.
4: Central Venous Catheter (CVC) Removal Procedures
The Art of CVC Removal
When the time comes to remove a central venous catheter (CVC), it’s crucial to follow established procedures to minimize patient discomfort, prevent complications, and ensure a smooth transition in the patient’s care.
Timing of Removal
Medical Evaluation: CVC removal is typically determined by the patient’s medical condition and treatment plan. A healthcare provider evaluates when it is safe and appropriate to remove the catheter.
Removal Technique
Gentle Extraction: CVC removal is a gentle, step-by-step process that begins with preparing the patient and the sterile field. The catheter is carefully withdrawn, and the site is assessed for any complications.

Site Closure and Aftercare
Closure Options: After catheter removal, the insertion site may be closed using sutures, skin adhesive, or steri-strips, depending on the specific circumstances.
Post-Removal Care: Patients receive instructions on post-removal care, which may include monitoring for any signs of complications and proper wound care.
Patient Education and Transition of Care
Empowering Patients: It’s essential to educate patients and caregivers about post-removal care, signs of infection, and any follow-up appointments or procedures needed.
Transition of Care: In cases where the removal of the CVC signifies the completion of treatment, patients may transition to other modes of care or monitoring as directed by their healthcare provider.
Mastering the art of CVC care, maintenance, and removal is a testament to the dedication of healthcare providers in ensuring patient safety and optimal treatment outcomes. By adhering to best practices and rigorous protocols, CVCs continue to serve as lifelines in the journey to improved health and well-being.
Navigating Central Venous Catheters with Care and Precision
In the intricate tapestry of modern medicine, central venous catheters (CVCs) emerge as indispensable lifelines, connecting patients with essential treatments and therapies. As we conclude this exploration of CVCs—unveiling their types, placement, maintenance, and removal—it becomes evident that these medical devices are not just tools; they are pillars of patient care, demanding the utmost care and precision in their management.
Empowering Healthcare Providers and Patients
Our journey through the world of CVCs has illuminated the significance of these lifelines. Healthcare providers, armed with knowledge and guided by strict protocols, ensure the safe and effective use of CVCs. Their dedication to sterile techniques, proper dressing changes, and vigilant monitoring safeguards patients from complications and infections.
Patient-Centered Care
For patients, CVCs represent both hope and challenges. They are conduits to life-saving treatments but also require diligence in self-care and an understanding of infection prevention. Patient education, empowerment, and active participation in their care journey are pivotal to maximizing the benefits of CVCs while minimizing risks.